X-rays/MRI's Do Not Explain Your Pain
Mar 11, 2021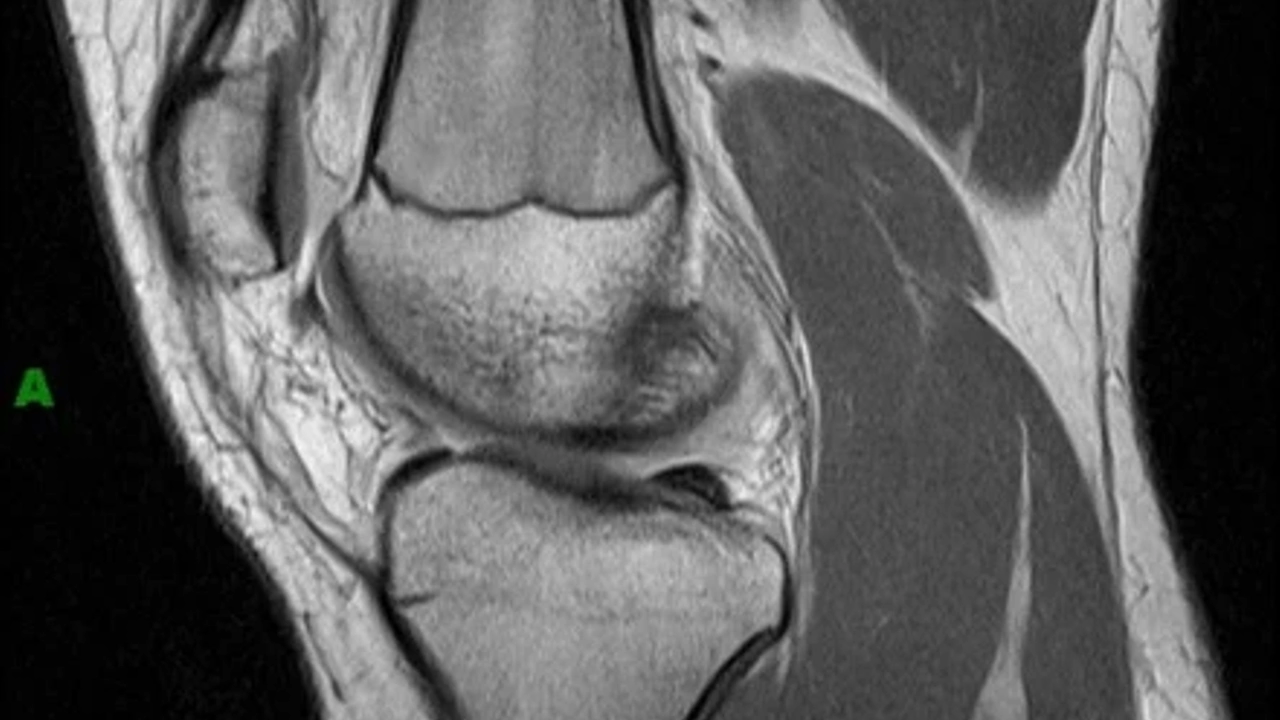
X-rays, MRI's, CT scans, etc. are incredible technological advancements in healthcare that allow the clinicians to visualize what is happening beneath the surface.
It gives precise identification of structural integrity, degree of tissue damage and can help guide recovery in some cases.
However, these scans cannot and do not explain pain and often times, there can be findings on a scan and you can be completely pain-free.
In one systematic review, they gathered data on the prevalence of MRI-confirmed degenerative spine conditions in asymptomatic individuals from 20 to 80 year olds. With a sample size of over 3,000 subjects they found the following:
"The prevalence of disk degeneration in asymptomatic individuals increased from 37% of 20-year-old individuals to 96% of 80-year-old individuals. Disk bulge prevalence increased from 30% of those 20 years of age to 84% of those 80 years of age. Disk protrusion prevalence increased from 29% of those 20 years of age to 43% of those 80 years of age. The prevalence of annular fissure increased from 19% of those 20 years of age to 29% of those 80 years of age." (1)
These findings imply that common diagnoses such as disc degeneration and disc herniations are both normal findings that are part of the normal aging process, as well as, findings that are often unknown and asymptomatic for most people.
Meniscal injuries are another common finding on MRI reports that often lead to patients believing they will need arthroscopic surgery to "clean out the knee" or even future total knee replacements. However, the incidence of asymptomatic meniscal tears is as high as 40-50%! That means, generally speaking, if you are in a room of 100 people, none of which are currently complaining of pain, about half of those people have some degree of a meniscus tear without even knowing.
So the questions that arise are:
1) Why are some people able to walk around without pain while other people have pain and swelling?
AND
2) How do we decide when surgery is actually necessary?
The answer to question one is simple: it all depends on how you are stressing the joint in question. Let's use the meniscus injury as the example. If you are able to properly and efficiently load and unload your knee (as well as all other joints), you will decrease the likelihood of putting excessive stress/torque/compression on the affected tissue. If we can avoid this excessive stress, we will avoid irritation of the joint, avoid constantly restarting the inflammatory process and avoid chronic changes to the structures in question.
The second question can be a little trickier. This should be a group decision including the patient, orthopedist and physical therapist (along with any other professionals who have been involved in the treatment of the patient). Conservative treatment through physical therapy should always be the first line of defense regardless of the MRI findings. Studies show that there is no significant difference in outcomes when comparing arthroscopic knee surgery for degenerative meniscal injuries with conservative treatment.(2)
In my opinion, attempting conservative treatment for 4 weeks is not a valiant effort. If you feel great after 4 weeks, excellent! If you don't, just be patient. Typically, movement patterns are engrained in us over the course of years or decades. If we want to make a meaningful change in how we are using our bodies and adapt a new, reflexive way of moving, it can take multiple months. If the alternative is to get cut into, then doing the same rehab for months after surgery, I elect not getting cut into.
Tendons, ligaments, bones and cartilage adapt and change relative to the stress we put it through. Everyone's daily activity and athletic activity is different and leads to a different stressor on their body. We can expect to see chronic, structural changes over time. Pain is complex. Schedule an assessment with a physical therapy to determine how you are moving and what type of stress you are putting on your body. X-rays and MRI's are great when we need them, but can lead to false expectations and fear avoidance if we do not understand the findings that may come up.
Want more information on what your x-ray or MRI means? You can contact me directly at [email protected] or comment below.
1. W. Brinjikji, P.H. Luetmer, B. Comstock, B.W. Bresnahan, L.E. Chen, R.A. Deyo, S. Halabi, J.A. Turner, A.L. Avins, K. James, J.T. Wald, D.F. Kallmes, J.G. Jarvik. Systematic Literature Review of Imaging Features of Spinal Degeneration in Asymptomatic Populations.
AJNR Am J Neuroradiol. 2015 Apr; 36(4): 811–816. Published online 2014 Nov 27. doi: 10.3174/ajnr.A4173
2. Lee DY, Park YJ, Kim HJ, Nam DC, Park JS, Song SY, Kang DG. Arthroscopic meniscal surgery versus conservative management in patients aged 40 years and older: a meta-analysis. Arch Orthop Trauma Surg. 2018 Dec;138(12):1731-1739. doi: 10.1007/s00402-018-2991-0. Epub 2018 Jul 4.
